Clinical Data Processing and Arrhythmia Source Detection
Clinical Data Files
These are examples of clinical data files. These files include 3D triangular mesh, catheter locations, electrograms, and others. Clinical data are exported from the mapping system. Atrium mesh and electrograms require further processing.
Atrium Geometry
This is how atrium geometry is created. As the catheter sweeps through the inside of the left atrium, the atrium geometry forms gradually.
This 3D triangular mesh often has defects, such as deep concave holes, intersecting triangular faces, non-referenced vertices, and more. An automated program was developed to process it. The refined 3D mesh contains no defects, and the size of the triangles is uniform.
Pulmonary veins and the mitral valve need to be cut. A user interface was developed for that. One pulmonary vein is selected, marked in blue, and then it can be removed from the mesh.
This is the algorithm for selecting a region of tissue. First, boundary vertices and a center vertex are selected. Then, the boundary vertices are linked to form the boundary line. Starting from the center point, the selection grows outward until it reaches the boundary, selecting all vertices inside. Selected vertices can be removed or new triangles can be filled in to flatten the region. The figures in the bottom row show the process of filling in new triangles, which removes spiky or deep concave regions.
Electrogram Noise Removal
Atrial electrograms often contain ventricle QRS interference. A QRS removal algorithm was developed. First, the median signal is subtracted from each electrogram. Then, QRS timing is identified on the 12 surface electrograms and refined using coronary sinus electrograms. Finally, around the QRS timing, QRS templates of the mapping catheter electrograms are created and subtracted.
These are examples before and after QRS removal. In figure (b), ventricle activations are removed while all atrium activations are preserved.
Activation Timing Detection
After electrogram noise is removed, an activation timing detection algorithm is applied. First, the original electrogram is processed, taking its absolute value, smoothing it, and finding rough activation timings. Then, around these rough timings, a median template of the electrogram is created. Next, cross-correlation between the template and the electrogram identifies peaks of the correlation coefficients. Long intervals are checked to determine if additional activations need to be added.
The figure below shows activation detection results.
Electroanatomical Mapping
Electroanatomical maps are valuable tools for guiding ablations. The process starts with patient data processing. From the electrogram, voltage, dominant frequency, fractionation, and synchrony can be derived. Activation timings are detected, providing local activation time and cycle length. From activation timing, an activation movie is created, enabling derivation of conduction velocity and phase singularity. These values can be interpolated to the atrium mesh and converted to color, forming a map.
Voltage map uses color to represent electrogram amplitude. Low voltage indicates scar. Scars conduct poorly, and complex scar distributions can lead to complex activation waves, making these regions targets for ablation. In this clinical example, a pulmonary vein isolation redo patient has regrown scars that require new ablations to recreate the line of block.
Local activation time map uses color to represent the sequence of activation. Normal activation originates from the Bachmann Bundle region. If the earliest activation site is elsewhere, ablation may be needed. In this clinical example, the focal source is marked in red, and ablations were performed there.
Although activation time maps are useful, they can be misleading. The choice of time window of interest dramatically affects the appearance of the map. Figure (a1) and (a2) show activation maps from the same activation, appearing very different due to differing time windows. Physicians look for red areas as focal sources, but the time window is not always optimal. A computer program only needs to find local minima, making what is invisible visible.
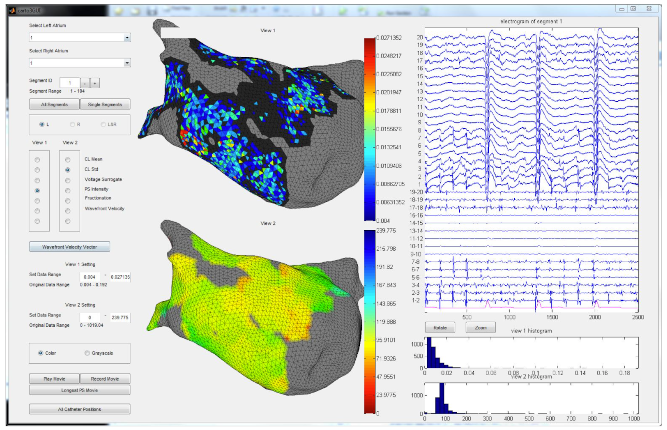
The system provides various ablation guidance maps. Multiple maps of different features help identify arrhythmia source locations. If several maps point to the same location, confidence is high that ablation at that location can terminate the regional arrhythmia.
To display the analysis results, an interactive user interface was built.